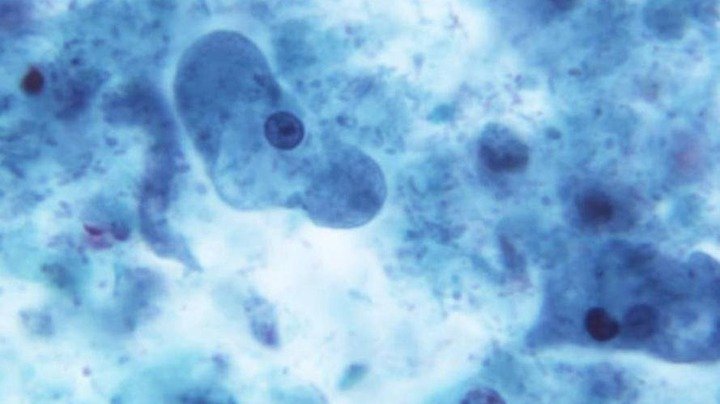
CDC
A recently published study led by researchers at Northern Arizona University (NAU) looked at the potential effects of a pan-resistant strain of bacteria. Antibiotic resistance is the term for when a particular type of antibiotic no longer works on a type of bacteria.
Lead author of the study Benjamin Koch, a senior research scientist at NAU’s Center for Ecosystem Science and Society (Ecoss), said many strains of bacteria are currently resistant to multiple kinds of antibiotics and pan-resistant bacteria — which are resistant to all known antibiotics — are developing.
“Pan-resistance is really an eventual certainty that our public health enterprise hasn’t reckoned with yet in terms of what this problem will actually look like,” he said, adding that the study was meant as a way to begin to address the gap.
Koch and other researchers at NAU began creating their model of what pan-resistant bacteria could mean for health in 2019. They published their findings in Communications Medicine on Dec. 26, 2024.
Ecoss director Bruce Hungate was a co-author the study, alongside researchers from the Milken Institute School of Public Health at George Washington University and the University of Minnesota. The researchers used data on a multiresistant strain of E. coli as the foundation for their model of a pan-resistant strain of the bacteria — which does not currently exist.
The focus on E. coli is because it’s a cause of sepsis, which Koch said kills about 350,000 people in the United States each year.
“The strain [that they modeled their research on] was not even detectable prior to the year 2000 and quickly gained prominence among the panoply of E. coli strains that cause sepsis,” he said.
The researchers used information when the strain emerged, its growth since then and proportion of sepsis infections that are caused by that strain, using it in their model for a hypothetical pan-resistant strain of E. coli. They made assumptions about how a pan-resistant strain might differ by using mortality rates of patients who’d had a delay in getting antibiotics. Those with a longer wait before receiving antibiotics tended to have worse outcomes, Koch said, and infections caused by pan-resistant bacteria could be considered similar to an indefinite delay, because no available antibiotics would be an effective treatment.
The study’s most conservative model predicts a 1,700% increase in sepsis deaths within five years of this kind of pan-resistant strain emerging. This means that a hospital that currently has about 60 sepsis deaths a year would see more than 1,000, assuming all of the infections were caused by a pan-resistant strain. (Koch noted that sepsis is caused by a variety of bacteria as well as a variety of bacterial strains.)
While the study was not focused on how to respond to and prepare for pan-resistant bacteria, Koch outlined some approaches he thought would be necessary. These included preventing infections before they happen, minimizing inappropriate use of antibiotics in all contexts, as well as research to find and develop new antibiotics and reduce the effects of pan-resistance.
Koch said he thought it could be important to conduct similar research on other strains of bacteria.
“Similar modeling exercises for other pathogens would give clinicians, policymakers and the general public a more comprehensive preview of a post antibiotic world,” he said. “I think that’s important so that they can accurately prioritize antibiotic resistance in relation to the many other current public health problems.”


